

E-Edition, E-Edition, Volume 15-4
Published September, 2018
“Coconut oil is pure poison,” so claims Karin Michels, PhD, a Harvard professor during a lecture at the University of Freiburg, Germany. Is Dr. Michels correct? Is coconut oil poisonous? Let’s look at the science. read more
There have been many theories proposed to explain the incredible healing effects of oil pulling, but what exactly is it that makes oil pulling so effective? read more
There are thousands of health books covering a wide variety of topics ranging from diet and nutrition to exercise and physical therapies. Out of all of these books, which two or three books are the most useful? read more
Nellie Bly could be called America’s first female medical investigative journalist. She is best known for her undercover exposé of the infamous Blackwell’s Island Insane Asylum. read more
The last article in a five-part series by Dr. Fabian Dayrit. The government’s dietary guidelines still recommend limiting saturated fat consumption. New research has proven there is no risk to eating saturated fats and in particular coconut oil. read more
“Coconut oil is pure poison,” claims Karin Michels, PhD, a part-time professor at Harvard TH Chan School of Public Health. Her comments given in a talk at the University of Freiburg, Germany, sparked a media frenzy with headlines such as, “Coconut Oil is Pure Poison Harvard Professor Claims” appearing in newspapers and on the internet.
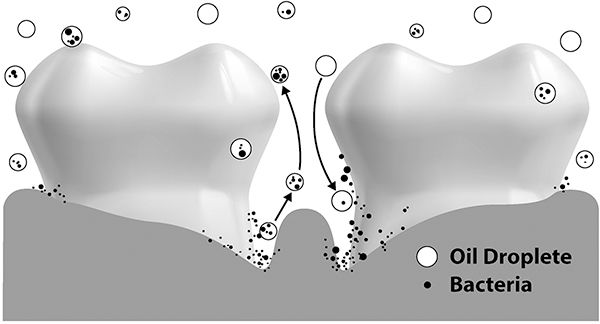
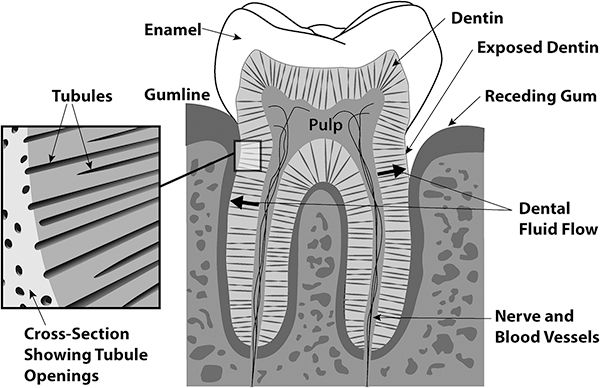
The sucking and swishing action of oil pulling creates a sucking force on and around the teeth, much like sucking on a straw. Bacteria hiding deep within periodontal pockets and within the tubules inside the tooth itself are drawn out. The flow of dental fluid through the tubules flushes bacteria out of these tiny canals where they are absorbed into the oil droplets and eventually are expelled from the mouth. In this manner, potential cavity-causing bacteria are removed from the inside of the teeth, as well as from deep periodontal pockets.
Oil Pulling Therapy
by Dr. Bruce Fife
Available from Piccadilly Books, Ltd.
for more information or to order click here
Oil Pulling Therapy
by Dr. Bruce Fife
Available from Piccadilly Books, Ltd.
for more information or to order click here
Ketone Therapy
by Dr. Bruce Fife
Available from Piccadilly Books, Ltd.
for more information or to order click here.
The Coconut Oil Miracle
by Dr. Bruce Fife
Available from Piccadilly Books, Ltd.
for more information or to order click here
Dr. Fife's Keto Cookery
by Dr. Bruce Fife
Available from Piccadilly Books, Ltd.
for more information or to order click here
Nelly Bly's was one of America’s most famous female journalists of the 19th century. She was a pioneer in the field of investigative journalism and was widely known for her writings about domestic servitude, political corruption, religious sects, baby-selling rings, swindlers, women’s suffrage, and worker’s strikes. She was a social crusader inasmuch as her editors allowed her to be. Bly was a mold-breaker in every sense of the word; she went places and did things that women had never done before, including her record breaking race around the world.
She traveled from New York to Europe, the Middle East, Southeast Asia, China, Japan, and across the American frontier completing the race in just 72 days beating her rival and establishing a world’s record. She later wrote a book chronicling her adventure, titled Around the World in 72 Days, which became a bestseller.
Around The World In 72 Days
By Nellie Bly
Available from Piccadilly Books, Ltd.
for information or to order click here
She often undertook investigative assignments that were part dare and part circulation booster. On another occasion, she posed as an unwed mother to unmask the baby-buying trade. Working for a time as a foreign correspondent in Mexico, she risked imprisonment for writing critical articles of the government, prompting her to flee the country. Later in her career, she served as a war correspondent during World War I and wrote stories about the Eastern front, some of which described the role of women in combat.
She was unable to convince the doctors she was not a lunatic and to let her free. Only with the aid of her editor was she able to escape and write about her harrowing experience trapped inside a madhouse. She later wrote a bestselling book recounting her experience titled Ten Days in A Madhouse.
Ten Days In A Madhouse
By Nellie Bly
Available from Piccadilly Books, Ltd.
for information or to order click here
The book provides an intriguing view into the way the mentally ill were treated a century ago. When it was released in 1887, it created quite a sensation, which led to a grand jury investigation and sweeping reform in the treatment of the mentally ill.
Key words: Ancel Keys, coconut oil, dietary guidelines, dietary fat-heart disease hypothesis
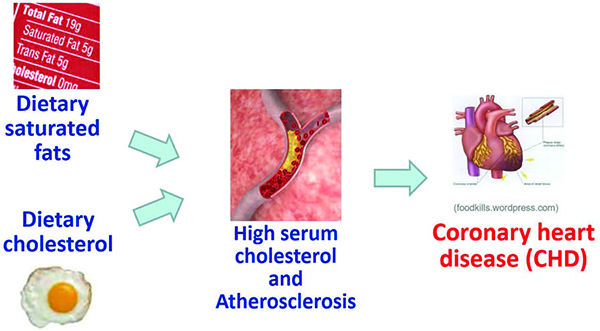
As early as 1965, the metabolic differences among the saturated fatty acids were already known. In a paper entitled, “Quantitative effects of dietary fat on serum cholesterol in man,” Hegsted and co-workers (1965) identified myristic acid (C14) and palmitic acid (C16), both LCFA, as primarily responsible for serum cholesterol. Nevertheless, Keys’ warning against all types of saturated fat, coconut oil included, remained.
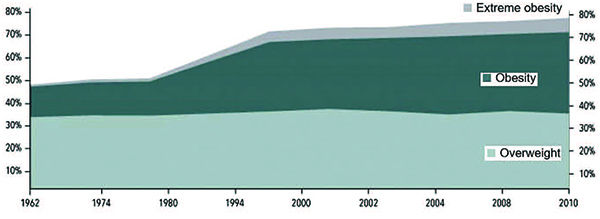
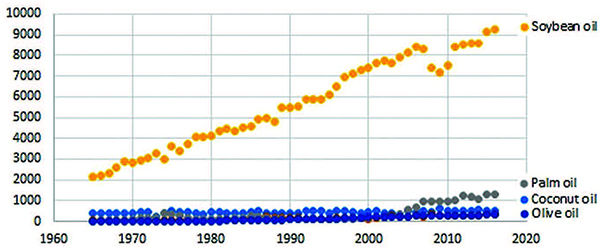
So what has been the result of the Dietary Guidelines for Americans? In 2010, 30 years after the first edition of the Dietary Guidelines, the Americans were overweight (37%), obese (35%) and extremely obese (6%). Since the early 1960s, the prevalence of overweight, obese, and extremely obese rose from 48% to 78% in American adults (Figure 2) (NIDDK 2012). It is noteworthy that there was a sharp increase in obesity beginning in 1980, the year the first Dietary Guidelines was published. Is this merely coincidental? Might there be a link between the advice being given by the Dietary Guidelines and this rise in the trend of overweight, obese, and extremely obese?
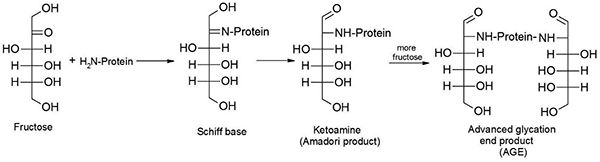
In addition, elevated levels of glucose and fructose in the blood stream are harmful because these compounds react chemically with proteins to form adducts called advanced glycation end-products (AGE) (de Vos et al. 2016). On the other hand, when polyunsaturated fatty acids (PUFA) are heated, they are oxidized and form degradation products, such as malondialdehyde, which also react with proteins to form AGE.
Recently uncovered industry documents reveal that the attacks on saturated fat and the promotion of sugar were part of a concerted campaign that was funded by the Sugar Research Foundation (SRF). As early as 1954, the SRF had identified a strategic opportunity for the sugar industry to increase market share by promoting a low fat (high sugar) diet and in 1965, it started strategically funding research projects by influential individuals. In 1967, the SRF paid $6,500 for two key review papers by McGandy and colleagues (1967a, 1967b). This campaign continues to the present time with the promulgation of pro-sugar policies by various international agencies (Kearns et al. 2016). In all of these policies, the recommendations have been always the same: take a low-fat diet and replace saturated fat with polyunsaturated fat. This is a dietary battle that continues to this day.
A partial release of the results of MCS study was made in a 1989 paper in the journal Arteriosclerosis with Frantz as lead author. This paper made the modest conclusion that: “For the entire study population, no differences between the treatment (high linoleic acid group) and control (high saturated fat group) were observed for cardiovascular events, cardiovascular deaths, or total mortality.” (Frantz et al. 1989).